Corresponding Author: Ferah Rehman, Department of Pediatric and Preventive Dentistry, Maulana Azad Institute of Dental Sciences, New Delhi, India, Phone: +91 8826246696, e-mail: drferahrehman@gmail.com
Objective: To scrutinize and consolidate treatment protocols and infection control measures to be practiced in pediatric dentistry during COVID-19 pandemic.
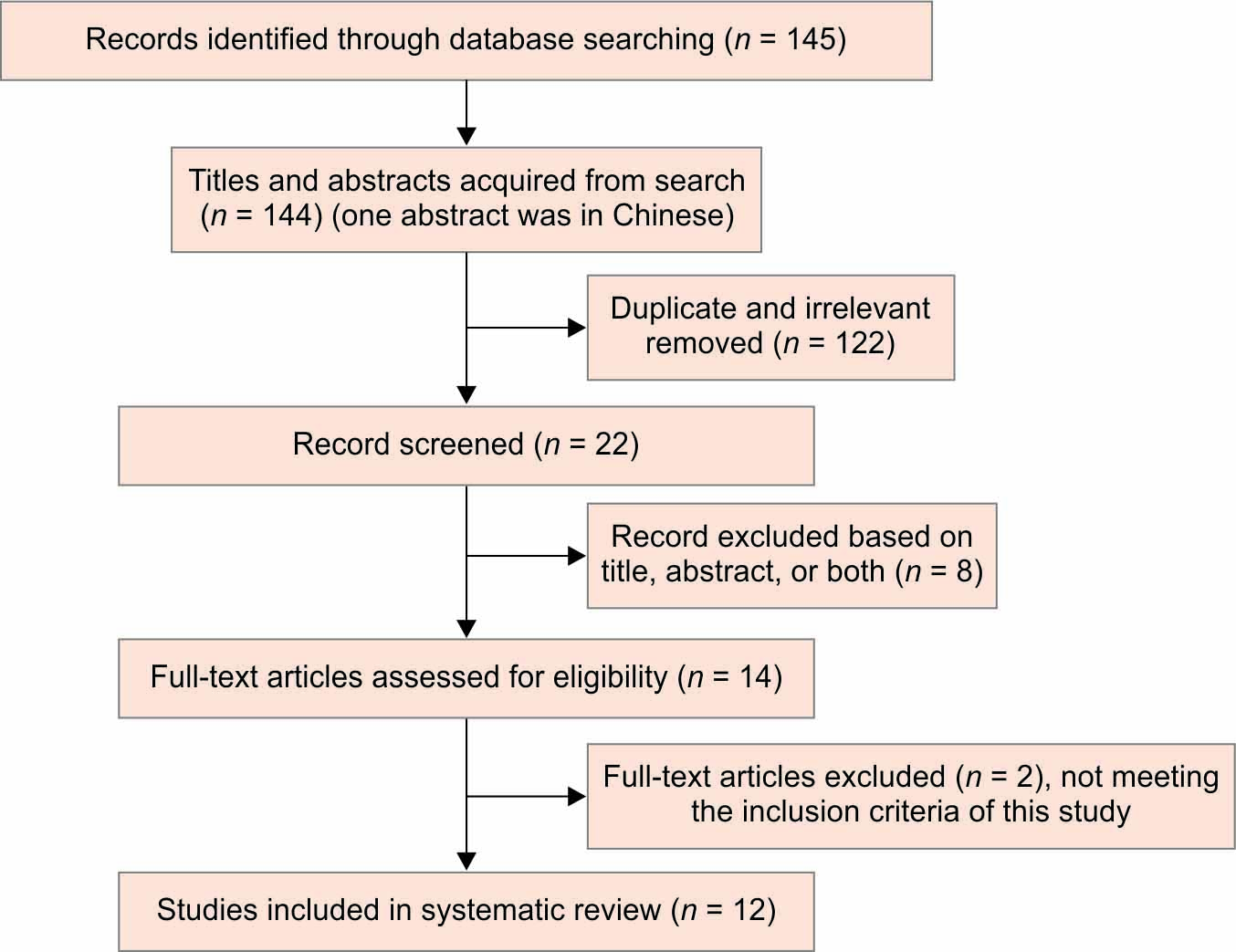
Study design: A systematic search pertaining to pediatric dental practice during COVID-19 was conducted using various electronic databases from 1st March to 31st July, 2020. The search resulted in a total of 145 records, out of which only 12 studies met our inclusion and exclusion criteria which were included in the present review.
Results: Data analysis was compiled under the following categories: Triage, waiting area and operatory changes, dentist’s safety, procedures to be undertaken during COVID-19, specific guidelines for trauma and children with special healthcare needs (SHCN) and infection control. Teledentistry, personal protective equipment (PPE), minimally invasive dentistry and non-aerosol-generating procedures are highly recommended. Urgent care should be provided to patients with dental traumaand SHCN. Surface disinfection and hand hygieneare considered important.
Conclusion: Transmission risk among children should not be overlooked and all the standard measures of prevention must be ensured in the pediatric practice.
How to cite this article: Kumar G, Yepes JF, Dhillon JK, et al. Guidelines and Standard Operating Protocol for Pediatric Dental Practice during COVID-19: A Systematic Review. J South Asian Assoc Pediatr Dent 2021;4(3):219-224.
Source of support: Nil
Conflict of interest: None
Keywords: COVID-19, Guidelines, Infection control, Pediatric dentistry.
Children infected with SARS-CoV-2 may show non-specific symptoms like fever, fatigue, headache, myalgia, cough, nasal congestion or rhinorrhea, loss of taste or smell, or may even be asymptomatic. Cough and fever, being the most common presenting symptoms. 1 , 3 A recent systematic review estimated that 16% of children with SARS-CoV-2 infection are asymptomatic, 4 but evidence from a French study suggests that as many as 45% of pediatric cases are asymptomatic. 5 The symptom-based screening for identification of SARS-CoV-2 infection in children is particularly challenging as there is lack of specificity of signs and symptoms and therefore all child patients and their parents should be considered as potential carriers. Literature suggests that the virus can spread from an infected person’s mouth or nose when they cough, sneeze, speak or breathe heavily when they spend long period of time with others in specific settings, particularly indoor, crowded and inadequately ventilated spaces. More evidence is required to better understand the conditions in which aerosol transmission is occurring outside of medical facilities where specific medical procedures, called aerosol-generating procedures, are conducted. 6 Transmission may also occur indirectly through touching surfaces in the immediate environment or objects contaminated with virus from an infected person, followed by touching the mouth, nose, or eyes. 7 This leaves rendering pediatric dental care at potentially high-risk when airotor is used producing aerosols at large quantity. Pediatric dentists must ensure current knowledge of local, regional, and national guidelines to optimize safety of children and accompanying parents. Further, in cases, where intervention is indicated, minimally invasive procedures that minimize or eliminate aerosol generation should be employed throughout the pandemic times, and in future, even when practice restrictions ease. Globally, numerous primary and secondary dental services have been suspended, with several countries providing telephone-based triage systems to identify those patients requiring urgent or emergency intervention. 8 , 9 Considering that pediatric dentistry has peculiarities related to the behavioral approach strategies and active participation of parents and caregivers, new guidelines or standard operating protocols are necessary and should be aimed at preventing and minimizing potential risk for both professionals and patients and caregivers during and after the coronavirus pandemic. 10 This systematic review is aimed to scrutinize and consolidate technical and scientific information available so far in order to minimize contamination risks in pediatric dentistry while imparting quality dental treatment to children during and after the COVID-19 pandemic.
This systematic review was reported according to the PRISMA checklist and was registered at the International Prospective Register of Systematic Reviews (PROSPERO) (protocol number # CRD42020191943).
A systematic search of the available studies in the literature was conducted using the following electronic databases: MEDLINE/PubMed, EMBASE, CINAHL, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, and SCOPUS from 1st March, 2020 to 31st July, 2020. The grey literature and the reference lists of identified full texts were also screened to retrieve additional relevant studies that might fulfill the inclusion criteria.
A search strategy was developed for the PubMed database which was followed with the other databases based on the following PICO question: “What Standard Operating Protocol and Guidelines has been developed for clinical management of Pediatric dental patients during COVID -19 pandemic?” The results of the different databases were manually cross-checked to locate and eliminate duplicate studies.
The complete search strategy included the use of text words and MeSH terms. The broad-based search was implemented individually with keywords: COVID-19 in Pediatric Dentistry, Coronavirus, SARS CoV-2, child oral health, pediatric dental setting guidelines, Standard operating protocols, modifications. Partial searches with the Boolean tools AND and OR were done with the above keywords individually with COVID-19 and Pediatric dentistry in different possible combinations. For additional details, the authors of the studies were contacted when required. The titles and abstracts were evaluated for suitability of inclusion in a systematic review. Two authors performed the literature search independently according to this predefined strategy.
The following inclusion criteria were used for study selection:
The following exclusion criteria were used for study selection:
A two-stage (title/abstracts and full-text) screening process with random pairs of independent reviewers was used. Disagreements between pairs of reviewers were resolved by discussion. The authors were contacted if additional information was necessary to determine eligibility. Only the data of interest within the selected studies were extracted for analysis.
One reviewer extracted data from high-quality literature and built evidence tables. A second reviewer checked the data that was extracted by comparing the extracted data with the data reported in the literature.
Tables were created to summarise the characteristics of the included studies, and any important questions related to the aim of this systematic review were recorded. All the published articles related to guidelines on pediatric dental clinical practice and COVID-19 was reviewed.
Two of the authors independently assessed the research quality and bias of each of the included articles using the relevant checklists from the Critical Appraisal Skills Programme (CASP). Any discrepancies between the review authors have been resolved by discussion, consulting a third review author.
The search resulted in a total of 145 records identified from the database. One of these was eliminated as it was in Chinese and the English translation was not available. The flowchart depicting the identification of records for this study is presented in Figure 1.
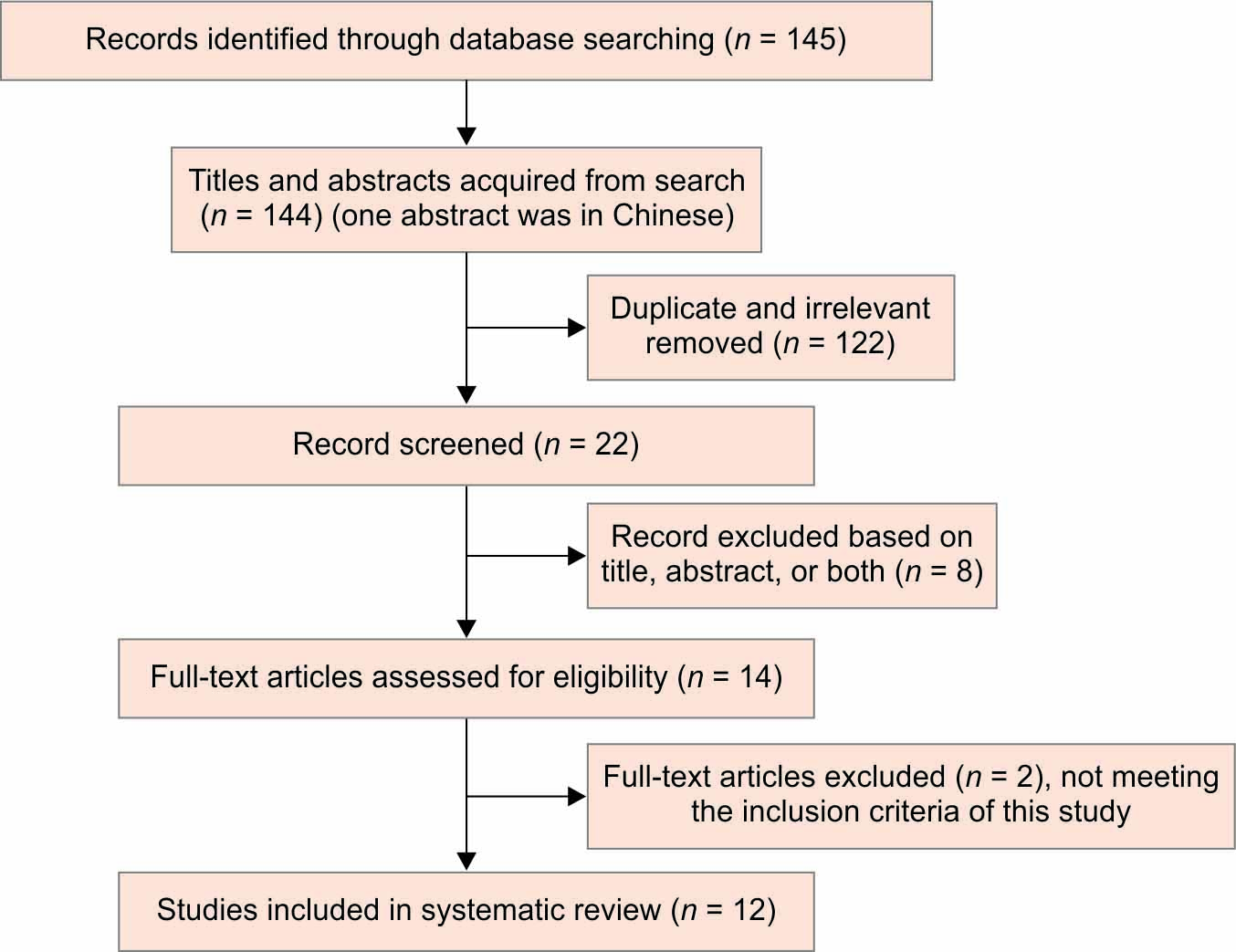
Fig. 1: Flowchart of the study articles
The results of the data analysis were classified into the following categories:
Triage, waiting area and operatory changes, dentist’s safety, procedures to be undertaken during COVID-19, specific guidelines for trauma/ guidelines for children with special healthcare needs, and infection control.
Mallineni et al. (2020), 11 Ferrazzano et al. (2020), 12 Ilyas et al. (2020), 13 Cianetti et al. (2020), 14 Al-Halabi et al. (2020), 15 de Amorim et al. (2020), 16 Jayaraman et al. (2020), 17 recommended triaging via Tele dentistry. In addition, Bahramian et al. 18 recommended that the temperature and SpO2 (oxygen saturation) of all patients should be checked before entering the clinic. Thermal scanning of patients while screening in the dental office was recommended by Ferrazzano et al. 12 and Cianetti et al. 14 . Obtaining a thorough medical history during triage including the history of recent travel was considered important. 19 , 21 Mallineni et al. 11 and Jayaraman et al. 17 recommended that all patients and parents should be considered as potential carriers of the virus.
Many authors recommended triaging the patients under emergent and non-emergent category and treating dental emergencies immediately while deferring non-urgent, elective care. 11 , 13 , 17
Social distancing in the operatory either by keeping the patients 2 meters apart or by staggering the appointments is recommended. Bahramian et al. 18 recommended provision of disposable shoe covers to patients and attendants. Hand hygiene using hand sanitizers and hand wash should be emphasized upon. Ferrazzano et al. 12 and de Amorim LM et al. 16 also recommended washing hands using soap and water. Some researchers recommended reducing the number of persons accompanying the patient for the appointment. 15 , 17 , 18 Bahramian et al. 18 recommended disinfection of seats, children’s toys, door handles, and faucets prior to the next patient. Al-Halabi et al. 15 and de Amorim et al. 16 suggested removing all unnecessary items from the waiting area. Al-Sehaibany FS 20 suggested that the toys in the dental office might be a potential source of infection. Patient education about hand hygiene should be provided as per some researchers. 15 , 16 , 19 One paper stated limited entry points to facilitate screening. 17
The use of PPE is highly recommended by all the authors. 11 , 21 However, there is no consensus regarding the type of PPE to be used with few authors recommended the use of N95 masks for all patients while others recommended the use of N 95 masks only for AGPs as depicted in flowchart.
All the papers included in the present review showed consensus for avoiding AGPs and the use of minimally invasive dentistry whenever possible. In addition, use of a pre-procedural mouth rinse is recommended. 12 , 19 , 21 Use of rubber dam, 14 , 15 , 18 , 19 use of high volume evacuation 12 , 13 , 15 , 19 , 21 to decrease aerosol generation is recommended.
Urgent care should be provided to patients with dental trauma 12 , 13 and patients with special healthcare needs. 12 , 15 There are limited suggestions regarding the type of interventions and continuing care in these patients during the pandemic.
Surface disinfection 11 , 14 , 16 , 18 , 20 , hand hygiene 11 , 19 are considered as important infection control measures. Reducing the risk of cross-infection with maintaining negative pressure in the operatory was recommended. 17 , 18 Other alternative to negative pressure is adequate ventilation 14 , 15 , 17 , 18 , 20 and HEPA filters. 14 , 17 Few researchers recommended the use of ultraviolet irradiation disinfecting system and air ionizer devices or ozone gas disinfection in the operatory. 18 , 20 One author recommended the use of air purifiers. 15 In addition, Jayaraman J et al recommended the rate of air change as ≥12 ACH for new and ≥6 ACH for existing rooms. In offices using nitrous oxide, disposable tubing should be considered. 15 Waste disposal should be done in impermeable and puncture-resistant bags 16 and potentially contaminated waste should be disposed of using the gooseneck ligation method for the waste bags. 19
Current research shows that children are physiologically just as likely to become infected with SARS CoV-2 as adults. 22 The discrepancy between the number of children infected and biological susceptibility may be due to the fact that children generally have minimal to mild symptoms when infected with the coronavirus and are therefore less likely to get tested. 23 A recent study from South Korea found that young children are less likely to spread the disease as compared to adults, while adolescents and teenagers between 10 and 19 years of age spread the virus at a similar rate as adults do. 24 Cruz and Zeichner have also suggested that children have a role in community-based viral transmission. 25 They noted that children are more likely than adults to have upper respiratory tract involvement with prolonged respiratory and fecal shedding. 26 The transmission from children in dental setup is yet not established but as a pediatric dentist, we have to take standard precautions to hamper this spread. Several researchers 11 , 21 have given different standard operating protocols to be followed in pediatric dental set up with conflicting guidelines; therefore it is imperative to sort and consolidate these guidelines, which is done in the present review.
In order to halt the transmission of coronavirus from patients to oral healthcare providers and vice versa, it is fundamental to have evidence-based data on personal protective equipment recommendations for the dentist during various procedures, infection prevention and control in the healthcare facility and waiting area modifications to avoid the spread of fomites on inanimate objects. Traumatic dental injuries were one of the emergencies seen at the earliest in pre-covid times, so the present paper was aimed to know the guidelines followed today and changes during recent times.
To minimize the risk of exposure and community spread, it is critical to reduce physical walk-ins in the dental setting and this can be done effectively by tele-screening and triaging. Triaging is the process of determining the priority of patients’ treatment needs based on the severity of their condition. The majority of the studies included in the present review advocated tele triaging as suggested by various National and International organizations during the pandemic. 26 , 28 However, few studies did not mention triage protocol in contrast to what is suggested by evidence based literature. 20 , 22 Teledentistry can serve as a good alternative to face to face consultations during COVID-19 era.
As the most common symptom of SARS CoV-2 among pediatric patients is known to be fever and cough, temperature screening is recommended for all patients reporting to healthcare facilities. On the contrary, only two studies in the present review gave importance to temperature screening. 12 , 18 This finding of the present review may be attributed to the rising cases of asymptomatic patients reporting to the pediatric dental settings. Also, SpO2 should be recorded for every patient as it is seen in some asymptomatic patients; there is a sudden drop in oxygen saturation without any major symptom of the disease, known as happy hypoxia. Majority of the dental patients are asymptomatic, therefore, the dentist should be cautious regarding this hypoxic state as it might be an indicator of infection. None of the studies except one 18 have included SpO2 screening in their practice.
To avoid transmission through indirect contact of contaminated surfaces of various objects like toys, magazines, décor items, etc in the waiting area, all the researchers 11 , 21 stated in the present review to rather modify the area by removing unnecessary items and instead put signages for respiratory hygiene/cough etiquette and social distancing. Based on the results, it is recommended to facilitate social distancing by scheduling appointments in such a way that there is only one patient in the dental clinic at a time to minimize contact in the waiting room and only a single person with a child patient should be allowed. If the waiting room does not allow for appropriate “social distancing,” patients should wait in their vehicle or outside the facility. 14 Provision of alcohol-based hand rub, and no-touch receptacles in the waiting area is recommended. One must consider installing electronic door openers to limit touching the door handles frequently. Physical barriers in the reception area are recommended so that direct contact of front desk personnel with the patients can be checked upon. Environments should be well ventilated, preferably with open windows according to the result of the present review.
According to current evidence, respiratory droplets and contact routes are the typical modes of transmission of the COVID-19 virus between people. 29 Droplet transmission occurs when a person comes in close contact (within 1 m) with someone who has respiratory symptoms (e.g., sneezing or coughing) and therefore, at risk of exposing his/her mucosa (mouth and nose) or conjunctiva (eyes) to potentially infective respiratory droplets. Transmission may also occur through fomites in the immediate environment around the infected person. 30 The asymptomatic incubation period for individuals infected with SARS-CoV-2 has been reported to be 1–14 days and it was seen that those without symptoms can also spread the virus. 30 , 32 Dental care settings invariably carry the risk of SARS-CoV-2 infection due to the specificity of its procedures. The pathogenic microorganisms can be transmitted in dental settings through inhalation of airborne microorganisms that can remain suspended in the air for long periods, 33 direct contact with blood, oral fluids, or other patient materials, 34 contact of conjunctival, nasal, or oral mucosa with droplets and aerosols containing microorganisms generated from an infected individual and propelled a short distance by coughing and talking without a mask 35 , 36 and indirect contact with contaminated instruments and/or environmental surfaces. 37 In addition to the infected patient’s cough and breathing, when dental devices such as high-speed dental handpiece are used in the patient’s oral cavity, a large amount of aerosol and droplets mixed with the patient’s saliva or even blood are generated. Droplets and aerosols particles are small enough to stay airborne for an extended period before they settle on environmental surfaces or enter the respiratory tract. Frequent direct or indirect contact of dental professionals with human fluids, patient materials, and contaminated dental instruments or environmental surfaces makes a possible route to the spread of viruses. The majority of studies in the present review have advocated the use of PPE while doing any aerosol-generating procedures. Because air droplet COVID-19 particles are estimated to be 0.06–0.14 μm in diameter, 38 the most efficient masks are presumed to be FFP2/N95, FFP3/N99, and N100. In consensus with this, the majority of the studies have recommended N-95 or high level respirators for any aerosol generating procedures, if the need arise.
The use of minimal invasive dentistry like atraumatic restorative treatment, sealing in carious lesions using fissure sealants, silver diamine fluoride, selective caries removal, and the Hall Technique is suggested by all the papers unanimously. It is suggested that fluoride varnish can be sent to patients with high caries risk scheduled for preventive programs and parents are educated about how to use fluoride varnish properly. 18 Extractions should be preferred for primary teeth and extirpations with hand instruments followed by temperature restorations in permanent teeth in order to minimize aerosol generating procedures. In the context of SARS-CoV-2, various preoperational antimicrobial or oxidative mouth rinse formulations were recommended including 1.5% H2O2 with a contact time of 30 seconds, Povidone-Iodine with a contact time of 15- and 30-second in concentrations of 0.5%, 1.25%, and 1.5% while in general chlorhexidine was considered inadequate.39-41 Further, in vitro studies by DE Anderson et al. and Egger et al. supported the use of povidone-iodine against SARS-CoV-2.
Rubber dams can significantly minimize the production of blood and saliva contaminated aerosol or spatter, particularly in cases when high-speed handpieces and dental ultrasonic devices are used. It has been reported that the use of rubber dam could significantly reduce airborne particles in a 3-foot diameter of the operational field by 70%. 42 In agreement with, this all the studies have advocated the use of rubber dam whenever any AGP is to be performed. When a rubber dam is applied, extra high-volume suction for aerosol and spatter should be used during the procedures along with regular suction. 43
Human coronaviruses such as SARS-CoV-2, Middle East Respiratory Syndrome coronavirus (MERS-CoV), or endemic human coronaviruses (HCoV) can survive on surfaces like metal, glass, or plastic for up to a couple of days. 44 Therefore, contaminated surfaces that are frequently contacted in healthcare settings are a potential source of coronavirus transmission and strict infection prevention and control measures should be practiced. In the present review, various ways of infection prevention like negative pressure in the operatory, HEPA filters, ultraviolet irradiation, ozone gas disinfection are suggested. All the papers included in the present review have emphasized on following strict infection prevention protocols in accordance with their respective hospital regimens.
All authors give their full consent for publication.
Within the limitation of the present review, it can be concluded that transmission risk through children should not be underestimated as they present either with very mild symptoms or are usually asymptomatic but an obvious potential carrier of the virus. So, all the treatment protocols and standard measures of prevention presented herein must be ensured in the pediatric dental practice in addition to local and regional guidelines issued now and again.
1. Dong Y, Mo X, Hu Y, et al.Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. J Emerg Med 2020;58(04):712–713. DOI: 10.1016/j.jemermed.2020.04.006
2. Foster CE, Moulton EA, Munoz FM, et al. Coronavirus disease 2019 in children cared for at Texas Children’s Hospital: initial clinical characteristics and outcomes. J Pediatric Infect Dis Soc 2020;9(03):373–377. DOI: 10.1093/jpids/piaa072
3. Xu H, Liu E, Xie J, et al.A follow-up study of children infected with SARS-CoV-2 from western China. Ann Transl Med 2020;8(10):623.
4. Assaker R, Colas AE, Julien-Marsollier F, et al.Presenting symptoms of COVID-19 in children: a meta-analysis of published studies. Br J Anaesth 2020;125(03):330–332. DOI: 10.1016/j.bja.2020.05.026
5. Poline J, Gaschignard J, Leblanc C, et al. Systematic SARS-CoV-2 screening at hospital admission in children: a French prospective multicenter study. Clin Infect Dis 2020;ciaa1044. DOI: 10.1093/cid/ciaa1044
9. Brazil National Health System (Sistema Unico de Saude). [Internet]. Dental care during COVID-19 [cited 2020 Oct 11]. Retrieved from: http://website.cfo.org.br/wp-content/uploads/2020/03/COVID-19_ATENDIMENTO-ODONTOLOGICONO-SUS.pdf.
10. Meyer BD, Casamassimo P, Vann WF.An algorithm for managing emergent dental conditions for children. J Clin Pediatr Dent 2019;43(03):201–206. DOI: 10.17796/1053-4625-43.3.10
11. Mallineni SK, Innes NP, Raggio DP, et al. Coronavirus disease (COVID-19): characteristics in children and considerations for dentists providing their care. Int J Paediatr Dent 2020;30(03):245–250.
12. Ferrazzano GF, Ingenito A, Cantile T. COVID-19 disease in children: what dentists should know and do to prevent viral spread. The Italian point of view. Int J Environ Res Public Health 2020;17(10):3642. DOI: 10.3390/ijerph17103642
13. Ilyas N, Agel M, Mitchell J et al.COVID-19 pandemic: the first wave - an audit and guidance for paediatric dentistry. Br Dent J 2020;228(12):927–931.
14. Cianetti S, Pagano S, Nardone M, et al. Model for taking care of patients with early childhood caries during the SARS-Cov-2 pandemic. Int J Environ Res Public Health 2020;17(11):3751. DOI: 10.3390/ijerph17113751
15. Al-Halabi M, Salami A, Alnuaimi E, et al. Assessment of paediatric dental guidelines and caries management alternatives in the post COVID-19 period. A critical review and clinical recommendations Eur Arch Paediatr Dent 2020;21:543–546. DOI: 10.1007/s40368-020-00547-5
16. Amorim LM, Maske TT, Ferreira SH, et al. New post-COVID-19 biosafety protocols in pediatric dentistry. Pesqui Bras Odontopediatria Clín Integr 2020;20(Suppl. 1):e0117. DOI: 10.1590/pboci.2020.117
17. Jayaraman J, Dhar V, Moorani Z, et al.Impact of COVID-19 on pediatric dental practice in the United StatesPediatr Dent 2020;42(03):180–183.
18. Bahramian H, Gharib B, Baghalian A. COVID-19 considerations in pediatric dentistry. JDR Clin Trans Res 2020;5(04):307–311.
19. Singh V, Lehl GK, Talwar M, et al. The novel coronavirus and challenges for general and paediatric dentists. Occup Med (Lond) 2020;70(05):320–322. DOI: 10.1177/2380084420941503
20. Al-Sehaibany FS. Middle East respiratory syndrome in children. Dental considerationsSaudi Med J 2017;38(04):339–343. DOI: 10.15537/smj.2017.4.15777
21. Cagetti MG, Angelino E. Could SARS-CoV-2 burst the use of non-invasive and minimally invasive treatments in paediatric dentistry? Int J Paediatr Dent 2020;00:1–4. DOI: 10.1111/ipd.12679
22. Zimmermann P, Curtis N. Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J 2020;39(05):355–368. DOI: 10.1097/INF.0000000000002660
23. Kathryn Moffett-Bradford et al., Science alert [Internet]. Do children spread COVID-19? Paediatricians break down what we know so far. [cited 2020 Oct 11] https://www.sciencealert.com/paediatricians-explain-what-we-know-about-children-who-get-covid-19#
24. Park YJ, Choe YJ, Park O, et al.COVID-19 national emergency response center, epidemiology and case management team. Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emerg Infect Dis 2020;26(10):2465–2468.
25. Cruz AT, Zeichner SL. COVID-19 in children: initial characterization of the pediatric disease. Pediatrics 2020;145(06):e20200834. DOI: 10.1542/peds.2020-0834
26. Guidance for Dental Settings. [Internet]. Interim infection prevention and control guidance for dental settings during the coronavirus disease 2019 (COVID-19) pandemic. [cited 2020 Oct 11] Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html
27. Guidelines for Dental Professionals in Covid-19 pandemic situation. [Internet]. [cited 2020 Oct 11] Available at: https://www.mohfw.gov.in/pdf/DentalAdvisoryF.pdf/
29. Liu J, Liao X, Qian S, et al. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerg Infect Dis 2020;26(06):1320–1323. DOI: 10.3201/eid2606.200239
30. Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20-28 January 2020. Euro Surveill 2020;25(05):2000062. DOI: 10.2807/1560-7917.ES.2020.25.5.2000062
31. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223):497-506.
32. Guan WJ, Ni ZY, Hu Y, et al.Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med 2020;382(18):1708–1720. DOI: 10.1101/2020.02.06.20020974
33. Kampf G, Todt D, Pfaender S, et al. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 2020;104(03):246–251. DOI: 10.1016/j.jhin.2020.01.022
34. Chen J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect 2020;22(02):69–71. DOI: 10.1016/j.micinf.2020.01.004
35. Cleveland JL, Gray SK, Harte JA, et al. Transmission of blood-borne pathogens in US dental healthcare settings: 2016 update. J Am Dent Assoc 2016;147(09):729–738. DOI: 10.1016/j.adaj.2016.03.020
36. Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc 2004;135(04):429–437. DOI: 10.14219/jada.archive.2004.0207
37. Liu L, Wei Q, Alvarez X, et al.Epithelial cells lining salivary gland ducts are early target cells of severe acute respiratory syndrome coronavirus infection in the upper respiratory tracts of rhesus macaques. J Virol. 2011;85(08):4025–4030. DOI: 10.1128/JVI.02292-10
38. Zhu N, Zhang D, Wang W, et al.China novel coronavirus investigating and research team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382(08):727–733. DOI: 10.1056/NEJMoa2001017
39. Carrouel F, Conte MP, Fisher J, et al.COVID-19: a recommendation to examine the effect of Mouthrinses with β-cyclodextrin combined with Citrox in preventing infection and progression. J Clin Med 2020;9(04):1126. DOI: 10.3390/jcm9041126
40. Geller C, Varbanov M, Duval RE. Human coronaviruses: insights into environmental resistance and its influence on the development of new antiseptic strategies. Viruses 2012;4(11):3044–3068. DOI: 10.3390/v4113044
41. Gercina AC, de Souza Amorim K, Pagaduan R, et al. What is the best mouthrinse against Coronaviruses?Oral Surg 2020;13: DOI: 10.1111/ors.12549
42. Samaranayake LP, Reid J, Evans D. The efficacy of rubber dam isolation in reducing atmospheric bacterial contamination. ASDC J Dent Child 1989;56(06):442–444.
43. Samaranayake LP, Peiris M. Severe acute respiratory syndrome and dentistry: a retrospective view. J Am Dent Assoc 2004;135(09):1292–1302. DOI: 10.14219/jada.archive.2004.0405
44. Otter JA, Donskey C, Yezli S, et al. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. J Hosp Infect 2016;92(03):235–250. DOI: 10.1016/j.jhin.2015.08.027